Why AI still can’t solve the patient referral problem – and how it can do it – Healthcare Blog

Author: Naseem Noah
The call from the black hole
Three months into setting up Carenector's facility-to-facility platform, I received a call that pointed out all the issues with medical referrals. A hospital social worker, already using our personal patient platform to help families find care, has been working for six days to coordinate the institutional placement of an 82-year-old stroke patient. She has made 23 calls. 14 faxes were sent. The patient recovered but remained in an acute care bed that cost $2,000 a day because no one could identify which skilled nursing facilities had beds available, accepted her Medicaid, and had stroke recovery capabilities.
“I love the service you've created for your patients,” she told me, “but when I need to make transfers between facilities, I continue to use faxes. Can you fix that?” this Is the workflow the same? “
She was right. We're already in 2025, and despite billions of dollars invested in healthcare IT and artificial intelligence, referring patients often feels like it's 1995 again. Earlier this year, THCB editor Matthew Holt documented his attempts to get a specialist referral through Blue Shield of California. An echocardiogram referral sent by his doctor never reached the imaging center. When he needed a dermatologist, his medical team referred him to a provider, only to find out that the provider wasn't covered by his HMO plan at all. “There's a huge opportunity here,” Holt concluded after the long journey with offline systems, “even though we now have a lot of data … that can be put together and made useful for patients.”
In the United States, clinicians make more than 100 million specialty referrals each year, but studies show that as many as half are never completed.
Here’s what we’ve learned after one year of operation: We built a consumer-facing platform to help individuals and families find care providers that fit their needs, insurance, and location—it now serves more than 100 daily users, including patients, social workers, and discharge planners. But solving personal care search problems is only half the battle. Facility referral workflows—hospital to skilled nursing facility, SNF to rehab, clinic to specialist—remain beholden to fax machines and phone tags because no one is redesigning the actual coordination process.
That's what we're building now. The problem that troubles us is not Why don't we have better tools? it is Why have billions of dollars in investments in artificial intelligence left agency recommendation workflows virtually unchanged?
failed architecture
The answer doesn’t lie in smarter algorithms or shinier dashboards. It’s about the fundamental mismatch between how AI is deployed and how care coordination actually works.
Start with the data layer. One survey found that 69% of primary care physicians said they “always or most of the time” send complete referral notes to specialists, but only 34% of specialists said they received those notes. Even within a single hospital system, information often disappears at the handoff point. Matthew Holt experienced this firsthand when his physician's referral for an echocardiogram never reached the imaging center, despite having Blue Shield's prior authorization in the system.
But this fragmentation is more serious than a lack of recommendations. When Holt's medical team referred him to a dermatologist, they sent him to a provider not covered by the HMO plan, even though the EMR had his insurance information and member ID. As he documented, “There's a huge opportunity here… most of the data about who I should see… is available. It's just not obvious anywhere.” Medical groups, hospitals, and health plans each maintain their own systems, with no real-time integration to answer simple questions like: Is the provider in the patient's plan's network?
Then there's the issue of incentives. A 2022 evaluation of CMS' comprehensive primary care+ program found zero impact on decentralization of care. The researchers concluded that “highly fragmented care persists” because payment models do not adequately reward providers for truly closing the referral loop. No one gets paid to track down lost referrals, so referrals slip through the cracks.
Finally, there's a stubborn analog reality: more than half of referral handoffs still occur via fax (56%) or paper handed to the patient (45%). We haven’t redesigned workflows; we’ve just digitized the chaos.
Why “AI-driven” solutions keep failing
Given these issues, you might expect AI vendors to rush to market with solutions. Instead, most people make matters worse by viewing AI as an add-on rather than infrastructure.
Typical approaches: OCR scanning paper referrals, EHR field autofill widgets, risk score prediction algorithms. Each tool solves a micro problem but ignores the macro disaster. As an analysis by Innovaccer points out, healthcare AI risks “repeating the mistakes of the past, with disconnected tools leading to inefficiencies rather than solutions.”
A recent McKinsey analysis makes the same point: the widespread adoption of AI-powered point solutions “is creating new fragmentation issues.” The way forward is not more siled tools, but rather “assembling these capabilities into modular, connected AI architectures.” Without data interoperability, none of this matters. As Innovaccer puts it bluntly, “Without clean data, true interoperability is just a fantasy. Without interoperability, AI is just expensive noise.”
What we're building — Information from over 100 daily users
Our consumer platform taught us something important: When you give people (and the social workers who help them) a tool that meets their needs in real time, they will use it. Daily. More than 100 users now rely on Carenector to navigate post-acute care, rehabilitation services and specialist referrals based on their insurance, location and medical requirements.
But these social workers keep telling us, “This works great when I'm helping family members search on their own. But when I need to coordinate a discharge or facility transfer on behalf of my organization, I'm back in the Stone Age.”
That’s why we’re now building a facility-oriented platform, and we’re doing it differently than we did the first time. We don’t guess what hospitals need. We are actively testing it with a select group of partner agencies, combined with ongoing feedback from their case managers and discharge planners who already understand what works in the consumer product.
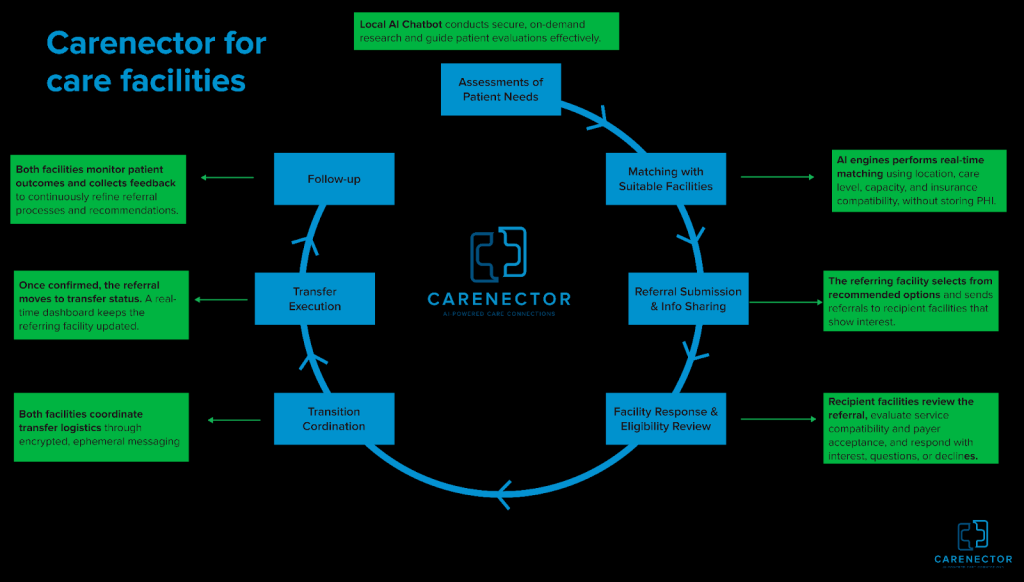
Facility workflow we are building
Rather than blending AI into the existing chaos, we’re rebuilding the agency referral process end-to-end. Care teams enter structured patient needs—diagnosis, recovery requirements, equipment, insurance type, location—without sharing any personally identifiable information. There are no names, no medical record numbers, and no dates of birth during the initial matching phase. Our AI engine performs real-time constraint-aware matching based purely on clinical and logistical criteria: If a patient requires skilled nursing care with PT services, is only on a specific Medicare plan, requires Spanish-speaking staff and must be within 10 miles, the system will only show facilities that meet all criteria simultaneously.
Once a match is found, the referring agency sends the query through a secure channel and both parties see the same status timeline. We established ad-hoc messaging threads where nurses and intake coordinators could communicate in real time, eliminating the need to fax to ineffective confusion. Once the agency accepts, everything comes together in one thread: shipping arrangements, medication reconciliation, and insurance verification.
Here’s the smart thing about it: we track whether a placement succeeds or fails. Was the patient readmitted within 30 days? Do the facility's services live up to their promises? The resulting data is fed back into the matching algorithm, which gradually learns which facilities deliver on their promises.
What we learn in real time:
We are building and testing this facility platform with a select group of partner hospitals and skilled nursing facilities. This is not yet widely available. We are iterating rapidly based on continued feedback from these early adopters, and these lessons are reshaping our approach:
- Trust requires transparency. Our early facility matching AI was a black box – “Trust us, these are great matches.” Adoption by our pilot partners was abysmal. When we add transparency display Why Each facility was matched based on specific criteria, and participation increased significantly. Case managers want to see the reasoning of the system, not just its recommendations.
- Privacy is about sensible defaults, not paranoia. We originally built to maximize privacy controls, which made the workflow unwieldy. Ongoing feedback from testing partners taught us the right approach: starting with zero PII during the matching phase, facilities only see clinical and logistical criteria. Use expired access and audit logs to share patient identifiers only after a facility indicates interest and capability. This middle path eliminates the referral black hole (where facilities can respond quickly without regulatory issues) while protecting patient privacy where it matters most.
- The real obstacle is not the technology, but the adoption strategy. One of the social workers in our pilot program has been sitting next to our test platform sending faxes. Three weeks into the test, after seeing four successful placements coordinated through our system, she stopped faxing. Technology hasn't changed. Her faith did it. We are learning that success is not measured by features released, but by workflows abandoned.
Beyond Technology: What Systems Need
Even the best-designed AI cannot solve the recommendation problem alone. Ecosystems require parallel changes:
- Regulatory reform: CMS may require electronic referral tracking as a condition of participation and pay providers for successful referrals, not just encounters.
- Standard adopted: The FHIR API and HL7 interoperability standards exist but are still optional. Forced adoption will allow systems from different vendors to truly communicate with each other.
- Shared Responsibilities: The biggest cultural shift required is from “I sent the referral” to “I confirmed the patient received care.” ACOs and value-based contracts are pushing in this direction, but progress is slow.
From Band-Aids to rebuilding pipes
The 82-year-old stroke patient? On the seventh day, she was placed via the social worker's fax machine. As a result of the delay, the hospital lost $14,000 in additional acute care days. Multiply that by millions of referrals per year and you see the economic waste embedded in our infrastructure.
The technology to solve this problem already exists – real-time data pipelines, constraint satisfaction algorithms, secure messaging, result analysis. We don’t yet have the will to reassemble the pieces into a coherent workflow rather than piling them onto a broken process.
Our consumer platform proves that when you rebuild the search and matching layer from the ground up, people will adopt it. We are now testing whether the same approach can be applied to institutional coordination with a select group of pilot facilities. The early signals from these partners are promising, and case managers using both of our products tell us that the facilities platform feels like a natural extension of the platform they already trust.
The most difficult conversations are not with engineers but with hospital administrators, who are overwhelmed by “artificial intelligence solutions” that promise transformation and expensive shelf space. We are no longer dominated by artificial intelligence. Let us first ask a question: When your case managers send a referral, do they know for sure that the referral has been received, reviewed, and acted upon? For most hospitals, the answer is no. That's what we're solving with our pilot partners.
If we succeed, it won't be because we build smarter algorithms. This is because we rebuilt the pipeline based on what real users told us they needed. What if we fail? This may be because we forget that technology has never been the hardest part of healthcare, trust is.
Naheem Noah is a doctoral researcher at the University of Denver and Kanektea medical referral platform.



