Officials said
New Orleans (AP) – Authorities say three of the 10 prisoners who escaped from New Orleans prison earlier this month were arrested in the woods for a week on Monday in two different states.
One of the men was arrested by local police and two other men in Baton Rouge, Louisiana, in Walker County, Texas, where the Louisiana Police Department posted Platform X.
Two more prisoners are still running, state police said. No other details about Monday's arrest were released immediately.
Authorities escaped the New Orleans area in the New Orleans area after jailbreak on May 16. The men pulled a defective cell door, opened a faulty cell door in the prison, squeezed into a hole behind the toilet, zoomed in to the dark coverage.
The prisoner's absence was not discovered until a few hours after they ran for freedom. The graffiti left on the wall contains the message of “simple lol” and the arrow points to the gap.
City and state officials noted that there were multiple security mistakes in the prison.
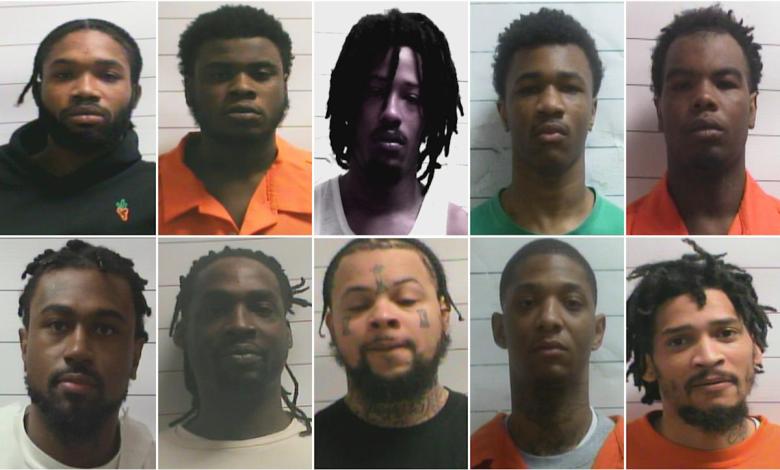
Louisiana authorities named the latest prisoners Renton Vanburran, Leo and Jermaine Donald. Prison Escape Dkenan Dennis, Corey Boyd, Gary C.
Many were initially in New Orleans prisons, awaiting a sentence or trial to charge violent crimes, including murder.
After escape, a prison maintenance worker was arrested and charged with turning off water to the toilet, and ACT authorities said the men helped the people leave. The worker said he was threatened by one of the prisoners if he refused to do so.
In addition, four others were arrested on suspicion of helping prisoners.


