Measuring the competitive environment through website neutral health insurance payments

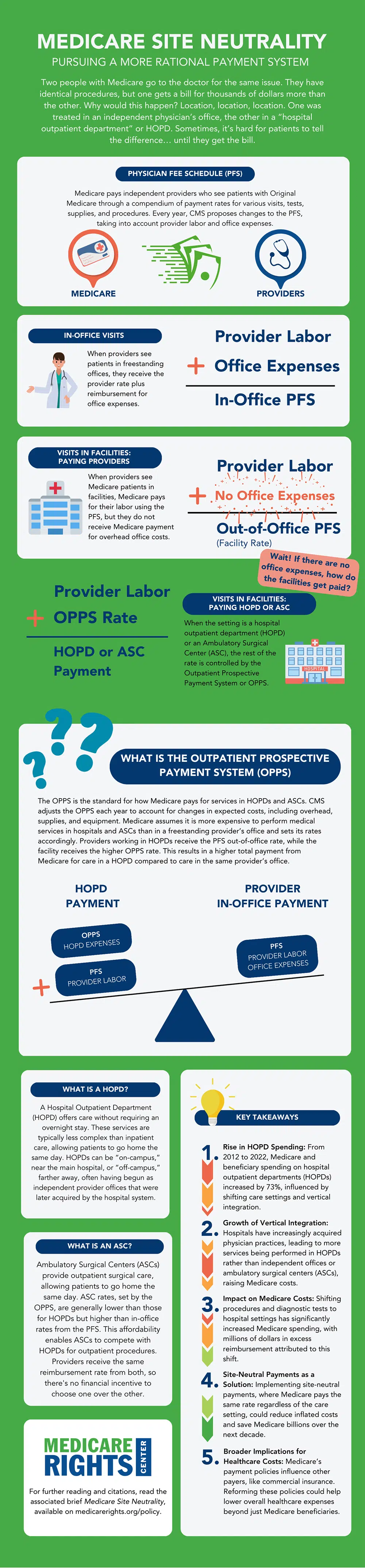
When Medicare pays for health services, there is a key factor that can lead to thousands of dollars in the same program as the same program: location. Where a person gets care and how to categorize that provider based on Medicare's payment structure is the hidden key. Medicare is usually paid for by the Hospital Clinic (HOPDS) than the Office of Independent Doctors, even if the services are provided the same. This provides hospitals with incentives to buy physician practices or use other strategies to transfer patients to more profitable websites. Over time, this drives taxpayer and beneficiary spending, resulting in financial stress on the health insurance plan.
Part 3: Medicare Website Neutral
The third and final part of the Medicare Rights Center series on Medicare Sustainability Policy examines the financial consequences of current location-specific payment rules and promotes a more reasonable payment system. Comparison of reimbursement rates for three categories of provider locations (No Dependence Physician Office, Outpatient Surgery Center (ASC) and HOPDS) Part 3 introduces policy directions for more sustainable payment systems for cross-clinical health insurance services.
Setting up unequal payments between
The Physician Fees Schedule (PFS) determines the costs of the clinician with original Medicare, including their labor and elevated office costs. When independent doctors see patients in independent offices, they receive PFS “office” rates. However, when the same care is provided in ASC or HOPD (both considered “facilities” under Medicare’s payment structure, the second set of repayment rules comes into play: outpatient expectation payment systems.
Practitioners working in these facilities receive “outdoor” PFS rates, PFS rates (part of the PFS of their labor costs), which receives office expenses from OPPS. This rate is much higher than the corresponding office reimbursement provided by PFS, and the ASC pays far more than the ASC than the standalone office and HOPD pays. This can result in a total bill of access to two to three times the same service clinicians provide in independent offices.
This means that hospitals have been motivated to purchase the practices of former independent physicians and integrate them vertically, refer patients to their hospital systems, and then drive traffic to the remaining independent practices and ASC. This number can be solved; HOPD services have expanded significantly and are taking up more and more Medicare outpatient spending. Spending on hospital outpatient services increased by 73% from 2012 to 2022, and as of 2022, hospitals had 53.6% of physician practices, a sharp increase from 38.8% in 2019. The narrow cost in the provider sector increases the cost of health insurance, taxpayers, beneficiaries and beneficiaries, making the hospital system pay and benefit from it.
Sustainability reform needs change initiatives
As stated in the first part of our Medicare Sustainability Policy Series, Part B outpatient services now account for the largest share of Medicare’s spending, and demand for Part B spending is only growing. Field neutrality is a crucial policy reform that will save savings in Part B spending – the Office of Government Accountability estimates that this change could save $141 billion over 10 years to ensure the same outpatient procedures are conducted to independent offices and hospital departments at the same interest rate. Ultimately, these solutions seek to improve payment accuracy and reduce overpayment by eliminating the economic incentives of hospitals to vertically integrate and absorb conventional care services that may be offered at lower costs.
Similarly, policy reforms against the spread of Medicare Advantage (MA) are outlined in the second part of our series, and also attempt to systematically reduce incentives that prompt insurers to flood the market in the MA program and to flood the market from the MA program and to profit from the overpayment. By statutes limiting the spread of programs and strengthening the public, federally funded consulting and information sources will enable people to make better coverage choices and avoid relying on biased information.
Ensuring Medicare’s sustainability requires policy-oriented changes to change the incentive structure of insurers and facilities. As long as the rules continue to allow overpayment and arbitrary cost inflation, the costs of health insurance and its services will continue to bear an increasing burden.
For more information on site neutrality, please see
Explore the infographic