The Overlooked Role of Tax Deductions in Roth Conversion Planning

Most discussions about Roth conversions focus on tax brackets and marginal tax rates. But before tax brackets come into play, there's another key factor that often determines how much you can convert in a given year: the tax deduction.
Understanding how deductions work with Roth conversions can help you make more intentional decisions, especially in years when your income is lower than usual. In some cases, the deduction can absorb your Roth conversion along with your other income during the year, resulting in an overall federal income tax owed of $0. This doesn't mean Roth conversions are always tax-free, but it can help you decide when it makes sense to convert and how much to convert in a given year.
That's why this part of the tax calculation is worth paying attention to before jumping directly to bracket-based strategies.
How Deductions Affect Roth Conversions
Before we dive in, it's helpful to understand how a Roth conversion shows up on your tax return. The mechanism is simple, but when incomes are lower, the impact of planning can be meaningful.
How a Roth Conversion is Taxed
When you complete a Roth conversion, the converted amount will be treated as ordinary income for federal income tax purposes. This income will be added to the rest of your taxable income for the year.
However, the first income is not taxed. Your income is deducted before federal income taxes are calculated, and then the remaining amount is taxed step-by-step across brackets.
planning opportunity deduction creation
Because deductions reduce taxable income before tax brackets apply, they effectively create a limited amount of income that can be absorbed each year without triggering federal income taxes.
In years when ordinary income is low, this deduction “room” can be intentionally exploited. A Roth conversion can fill that space, increasing taxable income on paper while keeping the total federal income tax owed the same.
This is not a special tax rule or loophole. This is simply the result of the deduction interacting with ordinary income on your tax return. The key is to recognize when the space existed and how much was available in a given year.
It’s easy to miss this planning opportunity when only considering tax brackets, which is why it helps to model directly.
Deduction Only Modeling in Boldin Planner
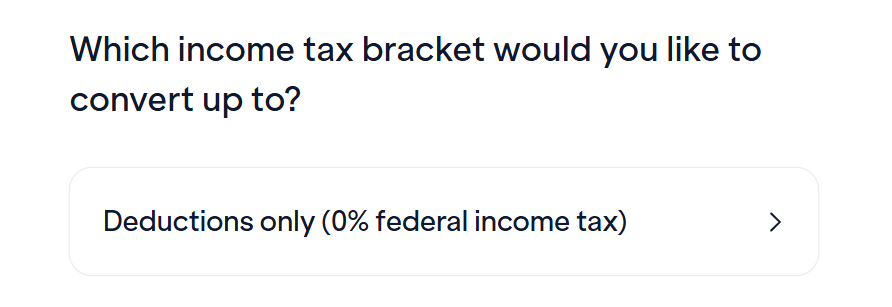
In Boldin's Roth Conversion Explorer, we've added a new “Deduction Only (0% Federal Income Tax)” strategy:
This strategy evaluates whether there is room left to absorb a Roth conversion after taking into account all other sources of income. The conversion still appears as income on your tax return, but the deduction is fully offset. Therefore, the total federal income tax owed remains $0. This is not a special tax bracket or loophole. This is simply a result of how the deduction offsets ordinary income on your tax return.
How different deductions create room for conversion
The source of the deduction is more important than the total amount available. Whether they come from the standard deduction, itemized expenses, age-based adjustments or pre-tax contributions, the planning concept is the same.
Standard deduction period
For tax year 2026, the standard deduction is $16,100 for single filers and $32,200 for married couples filing jointly.
This creates a base amount of income that is not subject to federal income taxes. If your total income is below that level, the extra income may be absorbed without triggering a tax. The Roth transformation may be an intentional way to use this space.
notes: Even if the deduction fully absorbs ordinary income, other types of income may be treated differently. Capital gains are calculated separately and may still be due even if federal income taxes remain at zero.
Additional deductions for ages 65 and over
If you are 65 or older, you may be eligible for a number of additional amounts to increase the amount of income you can absorb before federal income taxes apply.
The first is the existing age-based additional deduction standard. For tax year 2026, the amount is $2,050 for single or head-of-household filers and $1,650 for each qualifying spouse for married couples filing jointly.
Additionally, for tax years 2025 through 2028, current law provides for a temporary senior bonus deduction of up to $6,000 per individual and up to $12,000 for married couples filing jointly, subject to income limits and phase-out provisions. This bonus amount is separate from the age-based standard deduction and may further increase available room in qualifying years.
Taken together, these adjustments can significantly expand the amount of income within the range, particularly in the years before required minimum distributions begin. That's one reason why corollary-driven Roth conversion opportunities change significantly from year to year.
Year of itemized deductions
The same concept applies if you itemize deductions instead of taking the standard deduction.
Mortgage interest, charitable donations, and state and local taxes (SALT) can all increase your total deductions. In years when salt restrictions are expanded or itemized charges are unusually high, capacity may be greater than expected. This can create additional room for a Roth conversion even if there is no significant change in income.
The role of pre-tax contributions
Pre-tax contributions also affect this calculation. Contributions to accounts such as a traditional 401(k) or HSA reduce taxable income for the year.
By lowering taxable income, these contributions can increase the amount of Roth conversion income that qualifies for available deductions. That makes the space more dynamic than many expected, especially in years when contributions are unusually high.
When this approach usually makes sense
This strategy does not apply equally to all stages of life. It tends to occur during certain program windows when income is lower than usual.
Early retirement and low-income years
Retiring early before Social Security or required minimum distributions (RMDs) begin is a common example. During this stage, many people rely on brokerage accounts or cash to cover living expenses rather than earn an income.
For example, an early retiree might withdraw $75,000 from a brokerage account to cover living expenses during the year, with $60,000 representing long-term capital gains and the remainder coming from the cost basis. With little other ordinary income, they can also convert part of their traditional IRA to a Roth IRA, up to a standard deduction of $32,200 in 2026 (MFJ).
This deduction offsets the Roth conversion, leaving ordinary taxable income at zero. Since total taxable income remains within the 0% long-term capital gains threshold, capital gains are also taxed at 0%. The result is $0 in federal income taxes and $0 in capital gains taxes, even while financing living expenses and building Roth assets.
Career Changes and Contribution Years
This approach also works during career changes, vacations, or business slowdowns. In some years, pretax contributions alone can reduce taxable income enough to create unused deduction room.
The common denominator is that income is low relative to available deductions. When that happens, Rose's transformation may be worth exploring.
Where the Roth Long-Term Conversion Plan Deduction Applies
Deductions are not just about what they do this year, but how they affect taxes over time. Thinking of them as part of a broader Roth transformation strategy can help connect short-term decisions to long-term results.
Managing future tax stress
Tax-deferred retirement accounts are not going away. If money stays in a tax-deferred account, it will eventually be withdrawn and taxed. Over time, withdrawals can be stacked on top of Social Security and RMDs, pushing future earnings into a higher tax bracket than expected.
Taking advantage of deductions early can reduce your income facing this stress later on.
Provide flexibility for couples and survivors
For married couples, things often change when one of them dies. The surviving spouse will typically move into a higher tax bracket while living on a single income.
Converting some pre-tax funds early can reduce the income risk from higher interest rates in the future. This is particularly effective when deduction absorption is converted.
Use deductions as a starting point
Many people do Roth conversions by starting in their target tax bracket and working their way up. This framework can be useful, but it often skips previous steps.
The deduction generates a limited amount of income that can be absorbed each year before the brackets come into effect. If the space is unused, it will not be carried over. This specific approach helps make the space visible and provides a clear starting point before moving onto higher-level transformations.
The bigger picture
The goal of Roth transition planning is not the elimination of taxes but the thoughtful management of taxes over time. This means coordinating conversions with income, deductions, and long-term goals, rather than focusing on any one variable in isolation.
Roth conversion decisions can become clearer when this specific part of the tax calculation is considered part of the planning process rather than an afterthought. This clarity makes it easier for you to plan with confidence year after year. Over time, these small, intentional decisions can meaningfully increase retirement flexibility.
Use the Boldin Planner to help develop your Roth conversion strategy.
The post The Overlooked Role of Tax Deductions in Roth Conversion Planning appeared first on Bouldin.



